What Are the Stages of Heart Failure ?
Heart failure (HF) can be a misunderstood diagnosis. It describes a heart that is not pumping blood as well as it should, but it doesn’t mean the heart has “failed” or stopped working. There are different types of heart failure and different classifications used by healthcare providers to assess the stage and functional status of a person with HF.
Two classification systems
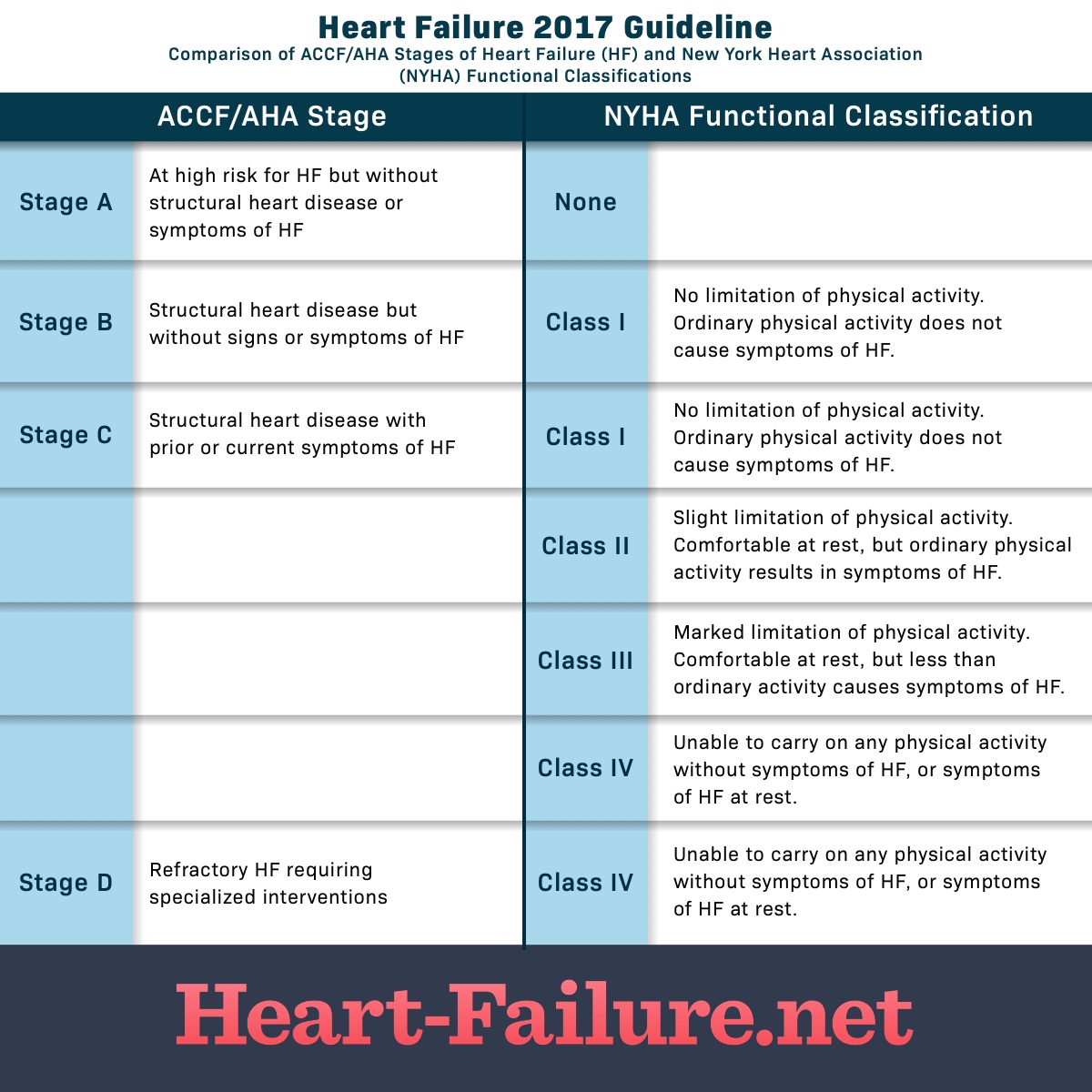
The American College of Cardiology/American Heart Association (ACC/AHA) has 4 stages of heart failure. The New York Heart Association (NYHA) Functional Classification labels functional limitations by class.
Healthcare providers usually classify a patients’ heart failure according to the severity of their self-reported symptoms. The most common classification system is the New York Heart Association (NYHA) Functional Classification. It uses four categories to differentiate people based on limitations during physical activity. The severity of their symptoms is compared to normal breathing, shortness of breath and pain as they interfere with or limit functioning during physical activity.
Research has demonstrated that classifying heart failure according to how well someone functions during physical activity, often called exertion, can be an important indicator of prognosis.
NYHA functional classification
The New York Heart Association (NYHA) classification system categorizes heart failure on a scale of I to IV:
- Class I: No limitation of physical activity
- Class II: Slight limitation of physical activity
- Class III: Marked limitation of physical activity
- Class IV: Symptoms occur even at rest; discomfort with any physical activity
The American College of Cardiology (ACC) and the American Heart Association (AHA) collaborated to create another classification system that complements the NYHA approach. It considers people who do not yet have HF but are at high risk for developing it.
ACC/AHA Stages
The American College of Cardiology/American Heart Association (ACC/AHA) staging system defines four stages:
- Stage A: High risk of heart failure but no structural heart disease or symptoms of heart failure (pre-heart failure)
- Stage B: Structural heart disease but no symptoms of heart failure (pre-heart failure)
- Stage C: Structural heart disease and symptoms of heart failure
- Stage D: Refractory heart failure requiring specialized interventions
Figure 1. Heart Failure stages and classes
The stages above describe the range from a high risk of developing heart failure on through advanced heart failure. The stages are correlated to treatment plans. The stages are also progressive, as HF worsens, you advance to the next stage of heart failure. There is no reversal through the stages. The objective is that with treatment, progression through the stages may be delayed.
What do the classifications really mean?
Heart failure is staged and classified by healthcare providers but what do they really mean. HF exists along a continuum. It can go from non-existent to mild to moderate to advanced, all over a period of time. Managing heart failure depends on the stage and can include the use of medications, lifestyle behaviors, and cardiac devices.
Mild heart failure may be evident when you experience minimal symptoms, such as shortness of breath, when involved in certain kinds of physical activity or maybe present without any symptoms. With early diagnosis, lifestyle changes, and medication, people with mild to moderate heart failure generally lead normal lives. Moderate heart failure is often classified along with mild HF. The same treatment approach is indicated.
Refractory congestive heart failure (CHF) occurs when symptoms continue to be present even after routine treatment. This is also called advanced heart failure or end-stage heart failure. It occurs when a person is not responding to or getting worse despite treatment.
Advanced or end-stage heart failure accounts for only about 10 percent of people diagnosed with HF. Patients with advanced heart failure can have symptoms at rest or with very little exertion. These include fatigue, dyspnea (shortness of breath), chronic coughing or wheezing, edema (swelling), nausea or lack of appetite, rapid heart rate, and sometimes confusion or impaired thinking due to a change in the balance of sodium levels in the blood.6 Advanced HF can be life-threatening. There are more aggressive treatment options including surgery that you can discuss with your healthcare provider to see if they are right for you. When there are no further treatment options, then patients are generally treated with palliative care. It is a time when the goal is to keep you comfortable, out of pain and minimize symptoms. There are numerous resources available to help with the many decisions to consider including hospice care, advance directives and other personal and legal matters.